The pelvic floor is a powerful yet sometimes overlooked part of the body. Made up of muscles, ligaments, and connective tissue, it plays a crucial role in stability, bladder and bowel control, and even sexual health. But when things go wrong, the impact can be life-changing.1
Pelvic Foor Dysfunction: Many Women Suffer in Silence
Although millions of women are affected by pelvic floor dysfunction (PFD), a true prevalence s is difficult to capture.2 The reason: PFD has a complex and multifactorial pathophysiology and encompasses a broad spectrum of clinical disorders - such as urinary incontinence, pelvic organ prolapse, fecal incontinence, and pelvic-perineal region pain syndrome.3 Thus, worldwide prevalences range from 1.9 % up to 46.5 %.3 But still many women do not report these issues, fearing stigma or assuming their symptoms are just “normal.”4
Did you Know? 3 Facts About PFD
Knowledge Gap: Many women have a gap in the knowledge of PFD, do not understand their treatment options, and are not able to identify risk factors for these disorders - that’s the authors’ conclusion of a literature review including 18 studies, comprising 11,512 women. Risk factors that were mostly related to lack of knowledge of PFD were educational level, access to information, socioeconomic status, age and race.5
Impact on Women’s Quality of Life: Given the range of problems PFD can cause, it’s no surprise that PFD can have a substantial impact on women’s quality of life. For example, a literature review found that 50-83 % of women with PFD report sexual dysfunction, compared to 30-50 % in the general population. Moreover, PFD may affect mental health: A case-control study revealed that women with PFD experience depression symptoms three times more often than those without.7
Genetics: While aging, obesity, and childbirth are well-established risk factors for PFD, research indicates that genetic and epigenetic factors may also contribute to PFD. Candidate gene and genome-wide association studies have identified e.g. susceptibility genes linked to pelvic organ prolapse and urinary incontinence. Genetic variants are thought to influence POP by impacting the stability of pelvic floor connective tissue.
Ultrasound for Faster Pelvic Floor Assessments
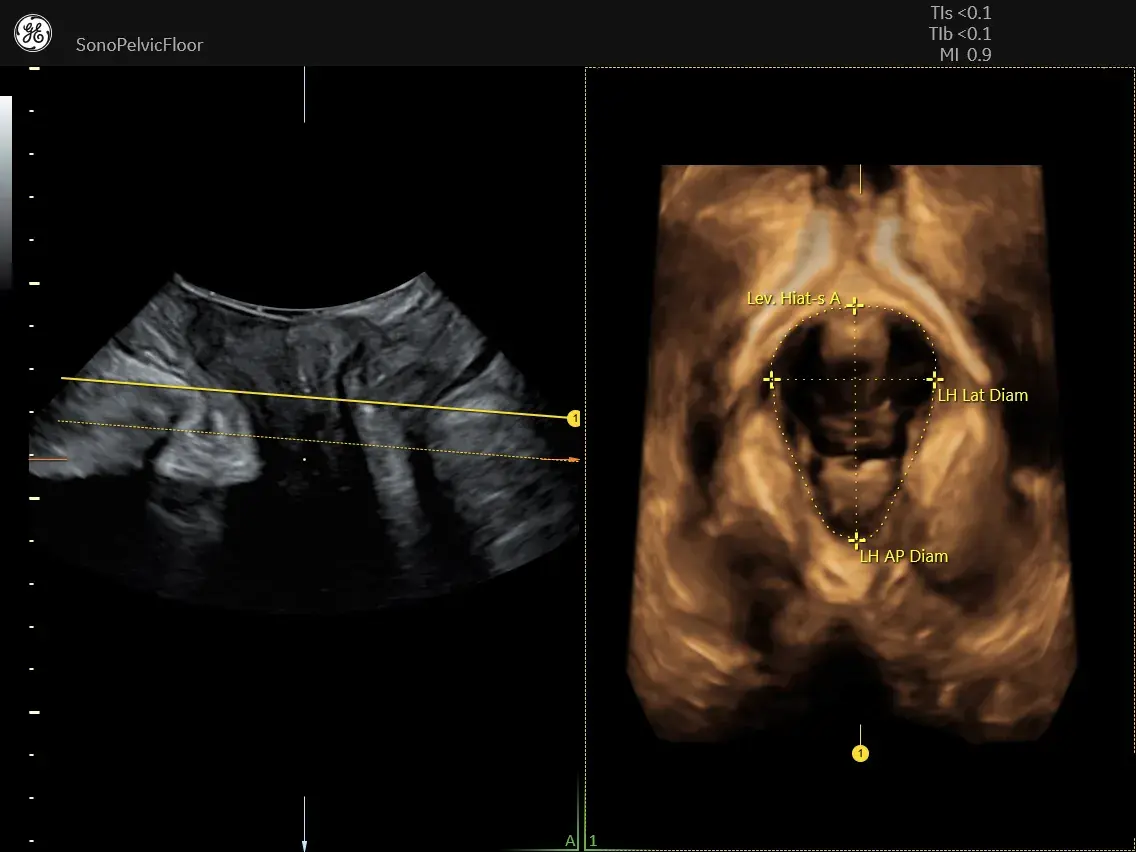
Analyzing pelvic floor anatomy can be complex, and physical examinations often have limitations.9 Alongside MRI and fluoroscopy, pelvic floor ultrasound is a key imaging modality for assessing PFD. It offers widespread availability, non-invasiveness, affordability, and real-time 3D imaging, providing clinicians with a detailed anatomic and functional roadmap for accurate diagnosis and treatment planning.
AI-powered technology can advance diagnosis one step further: SonoPelvicFloor2.0 streamlines exams with automated plane alignment, live C-plane tracking and measurements and offers a guided workflow for pelvic floor assessments. In fact, SonoPelvicFloor can reduce pelvic floor measurement exam time by 80% compared to manual exams.
Prioritize Precision with Ultrasound-Guided Diagnosis
Before starting treatment for PFD, an ultrasound-guided assessment can eliminate exam uncertainty and can provide more accurate measurements. Consider incorporating this technology to support confident, well-informed decisions in patient care.
Learn more about SonoPelvicFloor .
References:
- Tim, S. & Mazur-Bialy, A. I. The Most Common Functional Disorders and Factors Affecting Female Pelvic Floor. Life Basel Switz. 11, 1397 (2021).
- Kenne, K. A., Wendt, L. & Brooks Jackson, J. Prevalence of pelvic floor disorders in adult women being seen in a primary care setting and associated risk factors. Sci. Rep. 12, 9878 (2022).
- Peinado-Molina, R. A., Hernández-Martínez, A., Martínez-Vázquez, S., Rodríguez-Almagro, J. & Martínez-Galiano, J. M. Pelvic floor dysfunction: prevalence and associated factors. BMC Public Health 23, 2005 (2023).
- Rodríguez-Almagro, J. et al. A Qualitative Exploration of the Perceptions of Women Living with Pelvic Floor Disorders and Factors Related to Quality of Life. J. Clin. Med. 13, 1896 (2024).
- Fante, J. F., Silva, T. D., Mateus-Vasconcelos, E. C. L., Ferreira, C. H. J. & Brito, L. G. O. Do Women have Adequate Knowledge about Pelvic Floor Dysfunctions? A Systematic Review. Rev. Bras. Ginecol. E Obstet. Rev. Fed. Bras. Soc. Ginecol. E Obstet. 41, 508–519 (2019).
- Verbeek, M. & Hayward, L. Pelvic Floor Dysfunction And Its Effect On Quality Of Sexual Life. Sex. Med. Rev. 7, 559–564 (2019).
- Mazi, B., Kaddour, O. & Al-Badr, A. Depression symptoms in women with pelvic floor dysfunction: a case-control study. Int. J. Womens Health 11, 143–148 (2019).
- Lin, Y., Lin, Y., Zhou, X., Ren, A. & Li, X. Progress in the genetics and epigenetics of pelvic floor disorder. Gene 943, 149277 (2025).
- Ahmad, A. N., Hainsworth, A., Williams, A. B. & Schizas, A. M. P. A review of functional pelvic floor imaging modalities and their effectiveness. Clin. Imaging 39, 559–565 (2015).
- Bahrami, S. et al. Pelvic floor ultrasound: when, why, and how? Abdom. Radiol. N. Y. 46, 1395–1413 (2021).
JB01556AFG

 Clinical specialty
Clinical specialty










